Research Focus
Strokes claim more than 6 million victims annually. Survivors often experience a significantly reduced quality of life and undergo lengthy treatment, which is associated with serious social and economic consequences. The vast majority of cases are ischemic, i.e., caused by a reduction or complete blockage of blood flow to a specific part of the brain by a blood clot or atherosclerotic plaque. As the organ with the highest energy consumption, the brain is extremely sensitive to the cessation of nutrient and oxygen supply through blood circulation, so even a short period of ischemia can have fatal consequences. At the site of occlusion, where the tissue is affected by severe ischemic conditions, the fate of these cells is usually irreversible necrotic death (known as the ischemic core). The ischemic core is surrounded by tissue that is exposed to lower-intensity ischemia due to collateral blood supply (known as the “territory of risk” or ischemic penumbra). The penumbra tissue maintains reduced metabolic activity for a certain period of time and, after restoration of blood flow (or application of appropriate treatment), is able to reprogram the ischemic fate of cells and survive within this therapeutic window. The balance between the expansion of the infarct focus into the surrounding tissue and the ability of penumbra cells to survive defines the final extent of brain damage in stroke and, in fact, defines the effectiveness of treatment. Therefore, the penumbra has become the primary focus of our study, both in terms of the pathophysiology of the disease and testing the success of neuroprotective therapies.
The effectiveness of current stroke treatment in clinical practice has improved significantly in recent decades. Nevertheless, it is limited by early diagnosis and the start of treatment, but at the same time it is significantly influenced by the individual characteristics of the patient, such as age, gender, comorbidities, and body weight. In this context, there is a growing need for alternative experimental strategies and a personalized approach to their treatment. Our research is therefore primarily focused on:
- Studying the mechanisms of pathological transformation of ischemic-affected brain tissue with the aim of identifying potential innovative therapeutic targets.
- Developing, testing, and finding alternative uses for neuroprotective strategies at the experimental level.
- Defining potential modifiable and non-modifiable risk factors that reduce the success of neuroprotective therapies for ischemic brain tissue damage in order to personalize the treatment of patients with stroke.
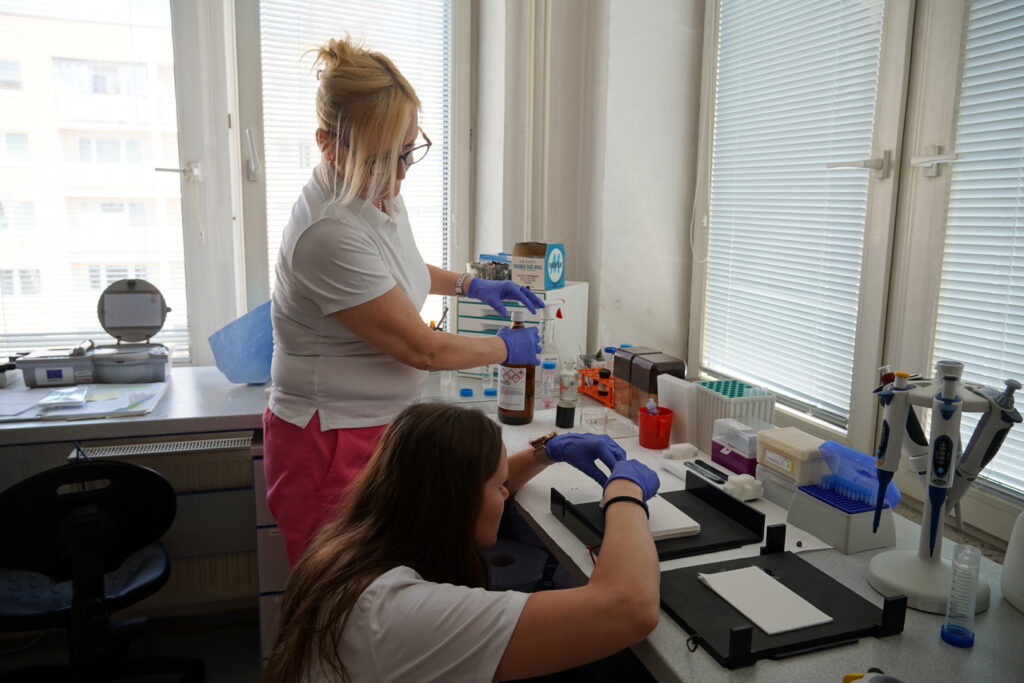
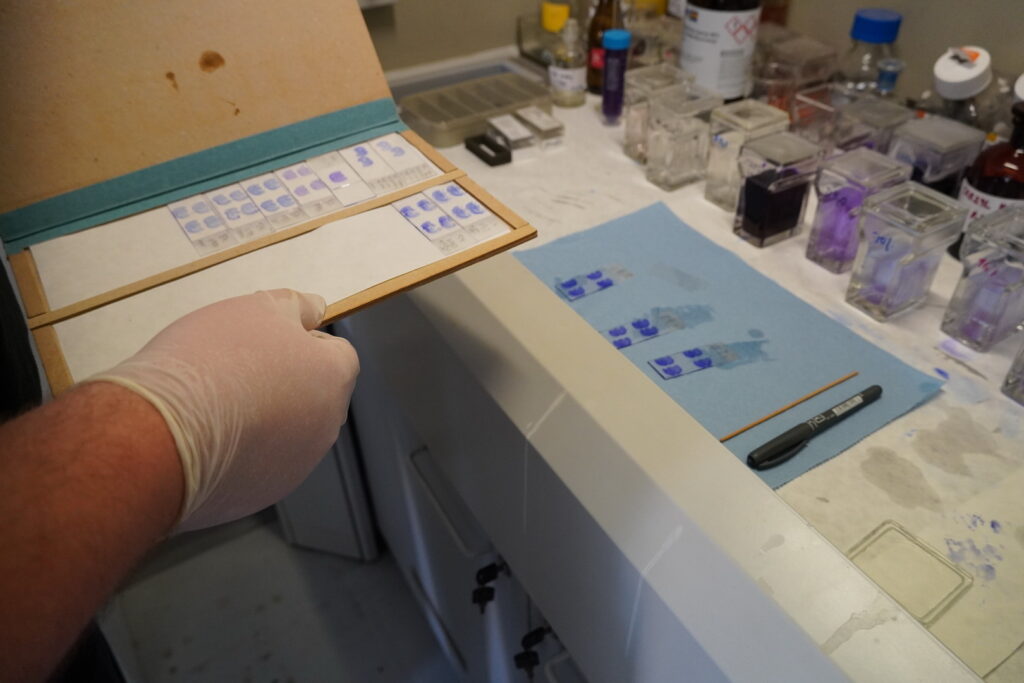
Photo Gallery



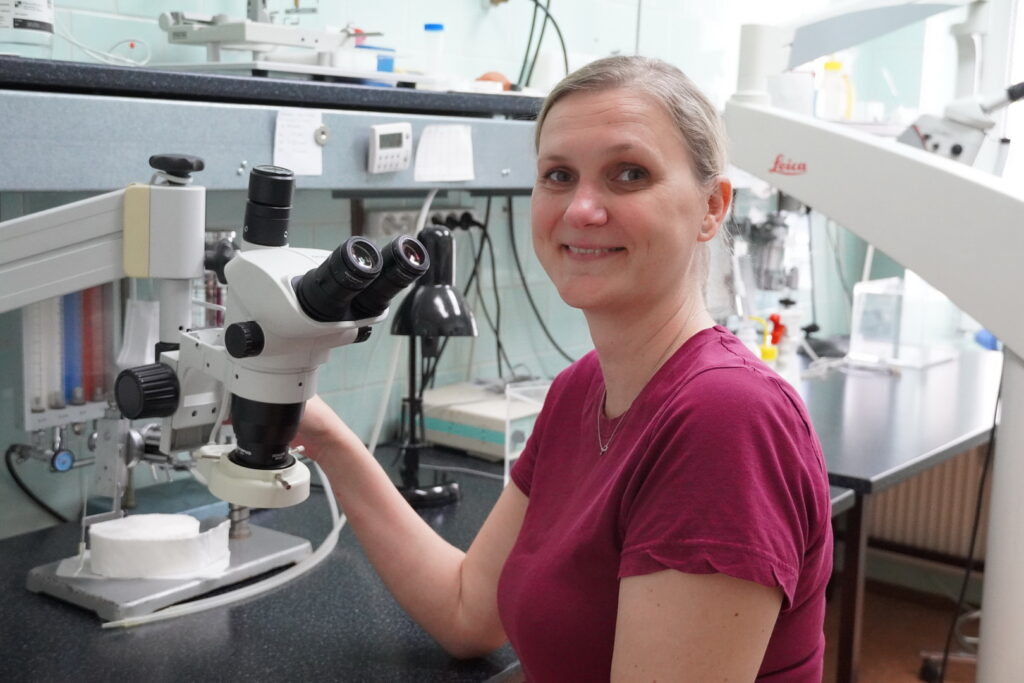
Head of the Research Group

Dr. Petra Bonová focuses on the mechanisms of ischemic tolerance after stroke, investigating the role of blood cells and paracrine factors in neuroprotection.
Employees
| Title | Name | Phone | ORCID | |
|---|---|---|---|---|
| RNDr., PhD. | 055/ 727 6226 |

|
||
| 055/ 727 6231 | ||||
| RNDr., PhD. |

|
|||
| RNDr., PhD. | ||||
| MVDr., PhD. | 055/727 6226 |

|


